WHITE PAPER
The Pharmacist’s Role in Addressing Social Determinants of Health
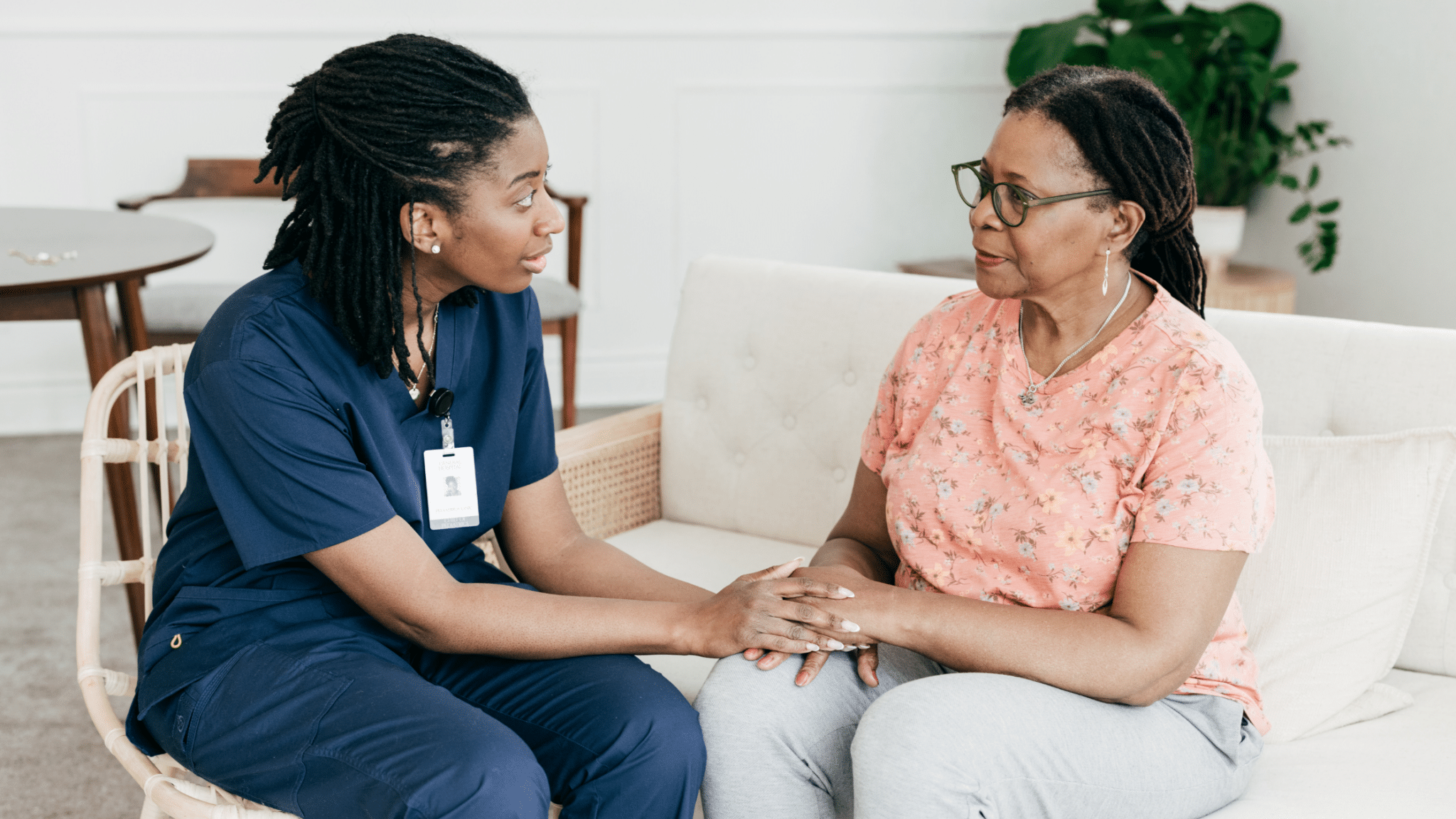
Table of Contents
Introduction
One of the more egregious – and heartbreaking – realities in today’s healthcare environment is the direct link between access to care and positive health outcomes. Officially, the conditions that stand in the way of healthcare access are called social determinants of health (SDOC), and include factors that are hard to control. Things like a person’s race, quality of education, economic security, or whether a person speaks English, or has access to public transportation. As the Centers for Disease Control (CDC) explains, “when people have limited access to resources they need to be healthy, they are more likely to experience health issues.”
Examples are everywhere. Adults who experience food insecurity are 2 to 3 times more likely to have type 2 diabetes. Children were found to be more than 19% more likely to suffer from asthma, and 28% more likely to experience depressive symptoms. The American Heart Association cites studies showing that food insecurity is associated with a range of adverse conditions including obesity, hypertension, diabetes, hyperlipidemia, and cardiovascular disease.
And that’s just food insecurity which according to the U.S. Department of Agriculture affects an estimated 13.5% of U.S. households, or almost 48 million people. Other examples include poor access to transportation, which affects about 15 million U.S. adults, making it difficult to reach doctors’ offices and other healthcare facilities. Another study found that individuals who do not complete high school were at a higher risk for reduced kidney function and cardiovascular disease.
As front-line healthcare providers, pharmacists see the effects of health inequities on a daily basis. Patients unable to afford medications due to sub-optimal insurance coverage, or no coverage at all. Patients with language barriers who can’t easily communicate their questions or concerns. Patients who don’t own a vehicle, and can’t easily travel to a pharmacy to pick up their medications or consult with a pharmacist. Or who can’t make it to the pharmacy during normal hours of operation.
Pharmacists can use their front-line role to help patients address the obstacles that preclude access to care. As members of their communities, pharmacists are attuned to the needs of their patients, and as trusted members of the medical profession, they are able to deliver critical assistance.
The following discussion will detail the many ways in which health disparities affect patient care, and offer insight about how pharmacists can help patients overcome those challenges.
What are Social Determinants of Health?
The CDC has identified several factors that disproportionately affect individuals’ ability to access the health-related resources they need. Collectively these factors are called social determinants of health (SDOH) and refer to the conditions in which people are born, raised, live, and work. Inequities in any of the following, the CDC notes, “influence health outcomes and quality of life.”

Social context refers to the human interactions where one lives, works, learns, plays, and worships. Special programs help protect the health and well-being of people who experience disadvantage. Social and community context also includes discrimination (the unfair treatment of people or groups based on their race, gender, age, or sexual orientation). Discrimination – including racism – can be found in many societal systems, including housing, education, criminal justice, and finance.
Expanding on this description, Tulane University’s Weatherhead School of Public Health & Tropical Medicine explains that social context also encompasses:
- Civic activities – voting, volunteering and participating in community groups.
- Social cohesion – solidarity between community members.
- Discrimination.
- Incarceration.
“People who participate in civic and community activities can make social connections, become more physically fit, and better manage mental health issues like depression,” the Tulane overview notes. “Consider how joining a bi-weekly tai chi or play-reading class at a local community center could improve a senior’s sense of belonging, or how volunteering at a food bank could help a depressed teenager feel a sense of purpose.”
Groups that have been marginalized face multiple barriers to accessing health care. Structural barriers including socioeconomic status, lack of insurance, transportation, childcare, or ability to take time off work to visit a doctor. Barriers to patient-provider interactions and health care quality also include cultural differences and language barriers.
Neighborhood and Physical Environment
Access to public transportation, supermarkets, and healthcare contribute to segregation of American cities. Discriminatory practices limit housing options to neighborhoods with inadequate funding for school districts, higher crime rates, poorly resourced infrastructure, and limited access to nutritious, affordable foods. These conditions can make illnesses, diseases, and injuries more common and severe among discriminated groups.
As an example, analysis by Deloitte cites a study of Los Angeles County, which found Black and Hispanic residents more likely than White people to live in pharmacy deserts. In addition to reduced access to pharmacies, the study found that pharmacies located in poor communities were 24% more likely to be out of stock or to have limited stock for the 13 most-commonly prescribed medications, and to have limited hours of operation.
Occupational health inequities are avoidable differences in work settings. Physical and mental health outcomes are linked to social, economic and environmental disadvantages. Other workforce factors include temporary work arrangements, socio-demographic characteristics (e.g., age, sex race), and organizational factors (e.g., lack of safety measures, limited or no health insurance).
In addition to lower-quality education, other barriers to good jobs include geographic location, language differences, discrimination, and access to transportation. Redlining (denying mortgages to people of color) also limits home ownership opportunity and ability to build wealth. Financial challenges make it difficult to manage expenses and access affordable quality housing, education, nutritious food, and reliable childcare.
Inequities in access to quality education commonly affect people who have been historically marginalized. Lower-quality education leads to lower literacy and numeracy levels, lower high school completion rates, and barriers to college entrance. Educational barriers limit future job options and lead to lower paying or less stable jobs.
Impact of Social Determinants of Health on Patient Outcomes

Health inequities put patients at risk for chronic conditions and serious illness. And they also add to the nation’s health spending tab. Analysis by Deloitte estimates that disparities add $320 billion annually to health spending, a figured projected to increase to a shocking $1 trillion or more by 2040. As an example, Deloitte cites the higher propensity for Black adults to be diagnosed with diabetes, and their ensuring experiences. “Racial inequity often contributes to a late diagnosis and comorbidities,” the analysis notes, “which results in $15 billion in unnecessary spending.”
Similarly, the study also found that of the $56 billion spent annually on asthma-related conditions, 4.3%, or $2.4 billion is considered “unnecessary spending associated with disparity.” Among other negative consequences, people at lower-income levels are more likely to receive a late diagnosis, and have trouble accessing needed care and medications.
The effects of health inequities run deep, with dire effects on affected communities. A list of more compelling impacts includes:
- Homelessness. People who experience homelessness are deeply affected by poor access to healthcare. One study of urban homeless identified drug overdoses as the top cause of death, and determined an average life expectancy of roughly 50 years, almost 20 years shorter than the non-homeless population.
- Among Black women, 9% are diagnosed with breast cancer when the disease is at an advanced stage, compared with 5% of white women.
- Colorectal Cancer. Black adults have a screening rate of 60% for colorectal cancer, compared with a 65% rate for White adults.
- Asthma. The overall asthma rate among children under age 19 years is 3.3%. But for children living below the federal poverty level (FPL) the rate is 5.4%.
- Cardiovascular Disease. A 10-year study among older Black, White, and Hispanic adults found that racial/ethnic segregation was linked to a 12% increased risk of cardiovascular disease compared with White adults.
- Pregnancy Risk. Research has shown significant racial and ethnic disparities in pregnancy-related mortality. As reported by the American Journal of Obstetrics & Gynecology (AJOG), “Black women have a pregnancy-related mortality ratio approximately three times as high as that of White women,” and during a study period that covered 2014-2017, Black women were three to four times more likely to die from pregnancy-related causes than White women.
- The AJOG study determined that Black, American Indian, and Alaska Native infants were more than twice as likely to die within the first year of life than White infants.
Unfortunately, this list is a small sample of the negative effects of health disparities on marginalized groups. A more comprehensive list would certainly continue for several pages and reveal the heartbreaking realities taking place within the U.S. healthcare system.
And while incidences of healthcare disparities are certainly not a new phenomenon, there does seem to be a heightened focus on addressing some of the underlying causes.
- The Affordable Care Act, signed into law by President Barack Obama in 2010, expanded healthcare coverage to millions of Americans and improved access to care, namely by offering incentives to states that expanded Medicaid eligibility.
- The American Rescue Plan, enacted in 2021 to provide economic relief from the effects of the COVID-19 pandemic, included several provisions aimed at social disparities. According to the JAMA Health Forum, key provisions include:
- Reducing child poverty through a new tax credit for children with families.
- Closing gaps in medical care by expanding healthcare coverage.
- Investing in community health centers and public health centers, and support for community mental health services.
- Increased funding for the federal food assistance program, the Supplemental Nutrition Assistance Program (SNAP), along with increased food assistance for school-age children.
- Funding for childcare and early education.
- Emergency housing assistance.
- Legislation introduced in the U.S. Congress in 2024, the Health Equity and Accountability Act (HEAA) targeted the health and wellbeing of underserved and marginalized communities with a comprehensive set of policy solutions. Among its key provisions, the legislation would improve access to cancer screening, expand federal funding of Medicaid, and offer universal free school lunch programs. The legislation, which was introduced in the last three sessions of Congress, has yet to be re-introduced in the current legislative session, which began in January 2025.
While the remedies mentioned above illustrate efforts at the federal level to address health inequities, other initiatives are being implemented across the nation. This includes offerings by state and local elected bodies as well as initiatives undertaken by business interests, community organizations, healthcare entities, and citizen groups. Addressing the multi-tentacled problem of healthcare disparity will require an “all hands-on deck” commitment from a wide swath of stakeholders, each of which can use their expertise to develop meaningful solutions. This includes of course, the nation’s pharmacists.
How Pharmacists Can Help
Patients can be excused for feeling the deck is stacked against them when it comes to healthcare access. This of course heightens the need for pharmacists to take a commanding lead in offering guidance, support, and solutions for the obstacles these patients encounter.
And make no mistake, pharmacists are responding to the challenge. A publication compiled by the Pharmacy Quality Alliance features multiple examples of actions taken by pharmacies nationwide to address SDOH-related issues. A few case study examples include:
- SDOH Screening. Pharmacists in Allegheny County, PA joined with the county health department and other community-based organizations to improve screenings, point-of-care testing and community service referrals among Black communities. During the initial pilot period more than 700 patients were screened, with 72% referred to other primary care or social services.
- Delayed Medication Pickup Outreach. Walgreens has initiated a “delayed pickup outreach” program whereby pharmacy employees reach out to patients who fail to pick up their medications nine days after the refill becomes available. Staff members contact patients to determine the reason the medication has not been picked up, and offer resources including free delivery, cost-related options, and assistance with transportation and literacy barriers.
- Special Considerations for Rural Communities. Healthwise Pharmacy in Hardin, Ohio offers special services that address barriers unique to rural communities. The pharmacy, which is affiliated with Ohio Northern University, initiated a home visitation service for patients with at least one chronic condition. Pharmacy staff review patients’ socioeconomic needs and offer critical services including medication therapy management (MTM), education, and if appropriate, point-of-care testing.
- Screening for Unmet Social Needs. Towncrest Pharmacy in Johnson County, Iowa, added a SDOH screening tool into its comprehensive medication review workflow. The screening is an 8-question verbal survey that pharmacy staff uses to identify unmet needs and make appropriate referrals.
As these impressive examples illustrate, pharmacies can – and are – making a difference. Other SDOC-related practices found throughout community pharmacies include:
Medication Accessibility and Affordability. Pharmacists can help patients address cost-related issues that can preclude accessibility to prescribed medications. This is an area in which technology, including the PrimeRx pharmacy management system, can be especially helpful. A few PrimeRx capabilities in this area include:
- Medication availability. Pharmacies can ensure medication accessibility through the PrimeRx Market online marketplace. Through PrimeRx Market, pharmacies have direct access to more than 40 drug wholesalers and suppliers. With just a few keystrokes a pharmacy can have a comprehensive listing of all suppliers that carry a required drug, along with detailed pricing information. Medication availability. Through PrimeRx Market, pharmacies have fingertip access to information about medication availability and pricing, and the ability to quickly locate – and purchase – patients’ required medications.
- Real-Time Prescription Benefit by Surescripts. PrimeRx pharmacies have direct access to the Real-Time Prescription Benefit solution which helps address medication accessibility and affordability. The solution seamlessly reviews a patient’s plan and determines if a prescribed medication is covered, and identifies out-of-pocket costs. Should a medication not be covered, or include a steep copay, the solution will identify less-costly therapeutic alternatives. In addition, if a medication requires a prior authorization, the solution will look for an alternative that does not require this time-consuming extra step.
- Coupons. PrimeRx identifies relevant manufacturer coupons and applies them at point-of-sale. The system determines if a patient is eligible for a particular coupon, and allows the patient to achieve immediate cost savings, right at the pharmacy register.
Patient Engagement. Pharmacists provide valuable assistance to patients by listening to their concerns and identifying social determinants of health during their conversations. As an example, the American Society of Health-System Pharmacists (ASHP) suggests a conversation about why a patient skips meals, exacerbating a diabetes condition, might reveal underlying food securities. The pharmacist can use this information to instruct a patient about care options and to provide referrals to appropriate social or healthcare agencies.
Medication Therapy Management (MTM). ASPHP suggests that MTM programs provide an important opportunity for pharmacists to have a role in health management. “MTM can be used to identify and resolve drug therapy programs,” the ASHP statement explains. “Pharmacists can develop comprehensive individual care plans, identify and meet vaccination needs, and improve health outcomes through adherence and management of chronic diseases.”
- Educational information. Pharmacists have access to informational brochures and handouts that can be shared with patients. This includes complementary materials produced by organizations including:
In addition, PrimeRx pharmacies can access an extensive library of patient education materials through integration with the Elsevier technology solution. Elsevier’s portfolio of solutions includes written handouts, health education videos, and medication/drug information sheets. Materials are available in multiple languages and are written in “user-friendly” format.
- Hotline Information. In addition to printed materials, many health and community organizations maintain hotline numbers that are staffed with trained professionals. Pharmacists should keep these numbers handy and make them available to patients in need of assistance. This includes state and local resources for food, transportation, housing, and utilities, as well as resources for mental health crises including substance abuse and suicide prevention.
Immunizations. As pharmacists can clearly attest, immunizations are powerful tools in protecting patients from major illnesses and have helped eradicate diseases such as polio and measles. But too many members of marginalized communities do not receive their recommended vaccines.
For example, current CDC guidance recommends that children receive vaccinations against 15 major illnesses by age 24 months. According to Northwell Health®, the CDC tracks administration of these vaccines though the “completion of the combined 7-vaccine series, a grouping of vaccines administered during the first two years of life that covers everything from polio and measles to hepatitis B.” However, the analysis notes, children living below the poverty line receive the 7-vaccine series at a significantly lower rate. While 68% of all U.S. children born in 2020 received their vaccines by age two, the completion rate was just 56% for children living below the poverty line. Further, the analysis that completion rates are higher among non-Hispanic White children, those with private insurance, and those living in urban areas.
Similarly, rates of influenza vaccination are significantly lower among low-income and minority communities, with the National Foundation for Infectious Diseases noting that while 54% of White Americans received a flu vaccine during the 2021-2022 flu season, only 42% of Black adults were vaccinated, and 38% of Hispanics.
With more than 90 percent of pharmacies offering some type of immunization services, usually anchored by influenza vaccines, pharmacists are well-qualified to help patients understand the importance of immunization adherence. Examples for improving patient engagement, offered by the CDC include:
- Education: Provide patients with educational information to dispel inaccurate information about vaccine safety and efficacy.
- Affordability: Patients without insurance may be eligible to receive free or low-cost vaccinations through their local community health service or state health department. Pharmacies can help patients identify opportunities, and if the administration site is not at the pharmacy, to make an appointment at the designated location.
- Communication. Systems including PrimeRx allow pharmacists to generate targeted email and text messages reminding patients about the importance of receiving recommended vaccines. For immunizations offered by the pharmacy, the email message can include a link that allows the patient to quickly schedule an appointment.
- Patient Counseling. The Department of Health and Human Services’ Healthy People report is the cornerstone of a federal initiative to improve Americans’ health and well-being. The current iteration, Healthy People 2030 includes nearly 360 measurable objectives, many of which fall under the purview of the nation’s pharmacies. Several recommendation for clinical preventative services, as outlined by US Pharmacist, include:
- Immunizations.
- Screening for alcohol use, anxiety, blood pressure, cervical dysplasia, depression, hearing, suicide risk, obesity, and vision.
- Smoking cessation.
- Fall risk assessment.
- Nutritional assessments.
- Community Referrals. As integral members of their communities, pharmacies are well-positioned to direct patients to the appropriate local or state social welfare or healthcare agency. Pharmacists will typically have relationships with local care facilities, and a good understanding of the services each facility offers. By sharing this information, pharmacies can eliminate the need for patients to look up this information on their own, which often results in a patient choosing to forego care.
Pharmacy eCare plans provide a standard format for pharmacists to use in documenting the precise services provided to patients, and to share that information with doctors, clinicians and other members of a patient’s health care team. With PrimeRx, pharmacists have direct access to this important tool, and an opportunity to further their role as care providers and ensure the highest levels of collaboration in patient care.
Conclusion
In May 2025, the World Health Organization (WHO) released a global report about the impact of social determinants of health on underlying causes of poor health. Among the report’s more alarming findings, was a significant reduction in life expectancy – sometimes by decades – in high-and-low-income countries. Specifically, the report found that people living in the country with the lowest live expectancy will, on average, live 33 fewer years than those born in the country with the highest life expectancy. 33 fewer years!
“Our world is an unequal one,” said WHO Director General Dr. Tedros Adhanom Ghebreyesus in releasing the report. “Where we are born, grow, live work and age significantly influences our health and well-being,”
Indeed, as this discussion has made clear, health inequities prevent millions of American from accessing proper care, often with heartbreaking consequences. Pharmacists though, can be a guiding light in helping people in their communities succeed by offering counsel, expertise and services.
References
“ASHP Statement on the Pharmacist’s Role in Public Health,” American Society of Hospital Pharmacies, 2021.
Baumgartner, Jesse C.; Collins, Sara R; and Radley, David C., “Racial and Ethnic Inequities in Health Care Coverage and Access 2013-2019,” Commonwealth Fund, June 9, 2021.
Choi, Andy; Weekley, Cristin; Chen, Shu-Cheng; Li, Suying; Tamura, Manjula Kurella; Norris, Keith; and Shlipak, Michael, “Association of Educational Attainment with Chronic Disease and Mortality: The Kidney Early Evaluation Program (KEEP),” August 2012.
Cooper, Lisa A., MD, MPH; Sharfstein, Joshua M., MD; and Thornton, Rachel L.J., MD PhD, “What the American Rescue Plan Means for Health Equity,” JAMA Health Forum, April 1, 2021.
Davis, Andy; Batra, Neal; Dhar, Asif; and Bhatt, Dr. Jay, “US health care can’t afford health inequities,” Deloitte Insights, June 22, 2022.
“Diabetes and Food Insecurity,” Centers for Disease Control, May 15, 2024.”
“Disparities in Flu Vaccination Coverage are Cause for Concern,” National Foundation for Infectious Diseases,” November 7, 2022.
“Education as a Social Determinant of Health,” Tulane University Celia Scott Weatherhead School of Public Health & Tropical Medicine, January 27, 2021.
“Food Security in the U.S. – Key Statistics and Graphics,” U.S. Department of Agriculture, January 8, 2025.
Grobman, William A., MBA; Entringer, Sonja, PhD; Simhan, Hyagriv, MD, MS; Yee, Lynn M., MPH; and Howell, Elizabeth A., “Social determinants of heath and obstetric outcomes,” Society for Maternal-Fetal Medicine, American Journal of Obstetrics & Gynecology, February 2024.
“Health inequities are shortening lives by decades,” World Health Organization press release, May 6, 2025.
“House and Senate Introduce Legislation Vital to Eliminating Health Disparities,” American Cancer Society press release, July 25, 2024.
Mowbray, Beth, “As more parents abstain from vaccinations, children from low-income households may pay the prices,” Northwell Health®, April 8, 2025.
“New Guide Helps Pharmacies Navigate Social Determinants of Health,” National Association of Boards of Pharmacy, April 5, 2022.
Ortaliza, Jared and Cox, Cynthia, “The Affordable Care Act 101,” KFF, July 29, 2024.
“PQA Social Determinants of Health,” Pharmacy Quality Alliance, April 5, 2022.
Rentz, Aleyna, “Unreliable Mass Transit and American Public Health,” Johns Hopkins Bloomberg School of Public Health, January 19, 2024.
Thomas, Margaret M.C., MWS; Miller, Daniel P., PhD; and Morrissey, Taryn W., PhD, “Food Insecurity and Child Health,” American Academy of Pediatrics, Volume 144, Issue 4, October 2019.
VanAntwerp, George, “The challenge of health equity in pharmacy,” Deloitte, July 2022.
“What is Health Equity?” Centers for Disease Control, June 11, 2024.
Yangbo, Sun, MD, PhD; Liu, Buyun, MD, PhD; Rong, Shuang, MD, PhD; Du, Yang, MS; Xu, Guifeng, MD; Snetselaar, Linda G., PhD; Wallace, Robert B., MD; and Bao, Wei, MD, PhD, “Food Insecurity is Associated with Cardiovascular and All-Cause Mortality Among Adults in the United States,” Journal of the American Heart Association, September 25, 2020.
Javed, Zulqarnin, MD, MPH, PhD; Maqsood, Muhammad Haisum, MD; Yahya, Tamer, MD; Amin, Zahir; Acquah, Isaac, MD, MPH; Valero-Elizondo, Javier, MD, MPH; Andrieni, Julia, MD; and Nasir, Khurram, MD, MPH, MSc, “Race, Racism and Cardiovascular Health,” Circulation: Cardiovascular Quality and Outcomes, January 2022.
Talk to an Expert!
With PrimeRx, pharmacy workflow tasks can be automated, leaving more time for pharmacists to engage with patients and focus on other pharmacy matters.

